Abstract
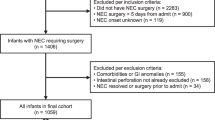
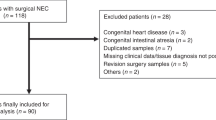
OBJECTIVE: To examine the increasing number of full-term infants at our hospital exhibiting necrotizing enterocolitis (NEC) in order to characterize these cases and to discover common risk factors.
METHODS: Medical charts were reviewed for all full-term infants (gestational age > 36 weeks) that were born in our institution during a 5-year period (from January 1, 1998 to December 31, 2002) and that developed definite NEC. Data regarding the rate of Cesarean section (CS) in our institution over the study period and five years prior to the study was also recorded.
RESULTS: During the 5 years of the study, 14 full-term infants were found to have NEC. The incidence of NEC in full-term infants increased from 0.16 to 0.71 per 1000 live births in the 5-year period. Mean birth weight was 2829 g. All the NEC infants except one were delivered by CS, and all of them were fed either with a mixture of breast milk and formula or entirely by formula. Seven of the infants (50%) had no major known risk factors predisposing them for NEC. Mean age of disease onset was very early (4.1 days) in most of the infants (12 infants), and the colon was the main NEC site. The short-term outcome was favorable in all but one case, which required explorative laparotomy for intestinal perforation. The number of infants born by CS has been steadily increasing, and was almost three times greater during the study period in comparison to the preceding years.
CONCLUSIONS: The etiology of NEC in the full-term population seems to differ from the etiology for the preterm group in its intestinal location and in the timing of its onset. The increase in the rate of CS over the years might be related to the concurrent increase in NEC, and this relationship should be further investigated.
Similar content being viewed by others
INTRODUCTION
The most important risk factor for necrotizing enterocolitis (NEC) is prematurity. Nonetheless, the incidence of NEC among the population of very low birth weight (VLBW) infants at our hospital has been decreasing over the years, as has the incidence of mortality and morbidity from this disease. Over the past 2 years, however, our hospital has experienced an increase in the incidence of full-term babies exhibiting NEC. NEC in full-term infants is well documented, accounting for about 10% of babies with NEC; it usually involves babies with known risk factors, such as intrauterine growth retardation (IUGR), birth asphyxia, congenital heart disease, gastroschisis, polycythemia, hypoglycemia, sepsis, exchange transfusion, umbilical lines, milk allergy, premature rupture of membranes with and without chorioamnionitis and gestational diabetes.1, 2, 3, 4, 5, 6, 7, 8 The purpose of the current study was to characterize this group of full-term infants with NEC, to discover whether there are any common known risk factors, and to review the relevant literature.
METHODS
Medical charts were reviewed for all full-term infants (gestational age > 36 weeks) that were born in our institution from January 1, 1998 to December 31, 2002 and that developed definite NEC. For the purpose of this study, only the files of those babies exhibiting Bell stage II and beyond9 were reviewed. For those babies, all relevant maternal and infant details were recorded, including details of maternal illnesses and drugs during and prior to the pregnancy, mode of delivery, birth weight, sex, Apgar scores, type of feeding prior to disease onset, bilirubin and hematocrit level, blood glucose levels, drugs or procedures administered prior to disease onset, other documented diseases, age at onset of first symptoms, abdominal X-ray interpretations, blood count and culture results, duration of clinical and radiological disease, and early and late complications as evidenced by rehospitalizations in our pediatric department.
No significant changes were made in terms of feeding patterns, percent of breast feeding in our nursery (70 to 80%), timing of feeding initiation after birth (4 to 6 hours) and type of formula given. No infection outbreaks or change in colonization were recorded during the study time period. There were no changes in obstetrical policies, such as epidural anesthesia or type of medications used (analgetics, antibiotics or other drugs) except for an overall gradual increase in the rate of CS. The incidence of infants who are small for gestational age remained the same in our institution, about 8%, over the study period.
The work-up on each of the infants in the study included complete blood count and blood culture, stool cultures for bacteria (Salmonella, Shigella, enteropathogenic Escherichia coli, Yersinia and Campylobacter) and viruses (enteroviruses and rota virus), blood electrolytes, and renal and liver function tests. Serial abdominal X-rays were taken until complete resolution of clinical and radiological findings. Feeding was resumed 7 days after normalization of abdominal X-rays. Each infant received intravenous cefotaxim and amikacin for a total of 7 days until cultures came back negative.
RESULTS
Table 1 shows that over the last 10 years, the incidence of NEC among full-term infants at our institution has increased, from 0. 16 per 1000 live births (full-term infants only) in 1993 to 0.71 per 1000 live births in 2002. This increase has been conspicuous mainly over the last 2 years, as shown in the table. The incidence of CS increased from 19% in 1998 to 24% in 2002 (in comparison to 14 to 16% in the previous 5 years). During the 5 years of the study, 14 full-term infants were found to have NEC. In this same period, the rate of NEC among VLBW infants born at our hospital decreased from 5.1% in 1998 to 2% in 2002. Maternal diseases observed in this group of infants included gestational diabetes, hypothyroidism and Turner's syndrome. All but one of the infants with NEC were born by CS, six due to nonreassuring fetal heart rate monitoring without apparent birth asphyxia (with one exception). The other seven infants were born by elective CS due to breech presentation, twin pregnancy or previous CS. As shown in Table 2, seven infants had known predisposing risk factors for NEC, such as growth retardation, polycythemia, congenital hypothyroidism, birth asphyxia, congenital heart malformation, and one infant with an as yet undiagnosed syndrome. The other seven infants either exhibited no obvious predisposing risk factors or had some common mild conditions, such as hyperbilirubinemia, early asymptomatic hypoglycemia and transient tachypnea. None of these infants was entirely breast-fed. The age of NEC onset in most of these babies was only a few days, except for two infants (N 2&4), with congenital heart disease and undiagnosed syndrome, respectively.
Nine babies had colon involvement, and in five babies, the radiologist was unable to unconditionally detect the exact location of the NEC. One baby was operated on for early perforation. All blood cultures were negative; in one case the urine culture was positive, and in one case Clostridium toxin was detected in the stool. All infants were discharged to their homes in good condition. During a 3-month follow-up period, two infants were re-admitted for obstructive ileus due to late-onset intestinal strictures that required explorative laparotomy with end-to-end anastomosis.
DISCUSSION
The incidence of NEC among full-term infants at our hospital has increased markedly over the last 5 years, while the incidence of NEC in VLBW infants has gradually decreased. The findings of the current study show that only half of these full-term infants with NEC exhibited known predisposing risk factors, including congenital heart disease, undiagnosed syndrome, birth asphyxia, intrauterine growth retardation and congenital hypothyroidism. Most of these infants had colon involvement, making this location typical among this group as compared to the preterm group, where the most common site is the jejunum and ileum.1 The early age at which the first clinical signs became obvious for most of the group is also unique as compared to reports for the preterm group, in whom the mean age of onset is 20 days of age.1
The incidence of NEC in infants with birth weight over 2500 g has previously been reported as 0.06 per 1000 live births, and about 7 to 25% of all NEC cases are term infants.1, 3, 10, 11 Over the last 5 years, a five-fold increase in the number of full-term infants with NEC was detected in our population, reaching an incidence of 0.71 per 1000 live births in 2002, equivalent to 58% of all NEC cases in our institution that year.
The clinical presentation of the infants at our hospital was similar to that described for preterm infants,1, 2 including abdominal distension, vomiting, bloody stools and septic appearance. We experienced no mortality among our group of patients, whereas the literature describes 5 and 12% mortality for full-term and preterm babies, respectively.10
NEC appears to occur earlier in full-term infants. In a case–control study of 43 full-term infants, Wiswell found the median onset of NEC to be only 2 days (18 developed NEC on the first day of life).12 Ruangtrakool studied 16 full-term infants; among them, NEC developed 8.6 days after birth, in comparison to 12.8 days after birth in preterm controls.13 Kabeer also found that NEC appeared earlier in a group of 20 full-term infants: at 5.3 days versus 15.3 days (in preterm infants).14 In the current study, the group mean age of NEC onset was 4.1 days among a group of 12 babies; however, for two other babies, one with congenital heart disease and the other with an as yet undiagnosed syndrome, NEC appeared much later, suggesting another pathogenesis.
The early age of onset may suggest a prenatal ischemic insult in six infants in the study group born by CS due to non-reassuring fetal monitoring, although without postnatal clinical signs of birth asphyxia (except one case). Another seven infants were born by elective CS. The possible relationship between increasing rates of CS and early NEC in full-term infants may be explained by the fact that sicker infants are saved by CS and by improved neonatal resuscitation. However, the low rate of birth asphyxia in the study group as well as the high rate of elective CS do not support such a hypothesis. So far, CS on its own has not been considered a risk factor for NEC by most authors, although Uauy et al.15 did mention CS as a significant risk factor in their group of VLBW infants with NEC. Recently, Minkoff and Chervenak16 discussed a possible mechanism by means of which the anesthesia involved in elective CS causes a possible transient drop of blood pressure, perhaps thus compromising placental blood supply and fetal circulation. In addition, the maternal supine position prior to and during the operation may further reduce fetal circulation and thus interfere with intestinal blood supply. The increasing incidence of CS in our institution may play some role in the higher incidence of NEC observed in this study. About 90% of all elective CS in our institution are under epidural anesthesia capable of compromising splanchnic blood supply to the fetus. This hypothesis should be further investigated by means of fetal Doppler blood flow measurements.
In the literature, proposed risk factors for NEC in term infants include cyanotic heart disease, perinatal asphyxia, hypoglycemia, polycythemia, respiratory distress syndrome, protracted diarrhea, pre-eclampsia, cocaine abuse during pregnancy, cows' milk allergy and anti-C Rhesus incompatibility.3, 4, 10, 17 One case–control study of 24 infants weighing over 2000 g at birth who developed NEC found a higher frequency of premature rupture of membranes, chorioamnionitis, Apgar score less than 7 for the first and fifth minute, respiratory distress syndrome, congenital heart disease, hypoglycemia and exchange transfusion, but no greater frequency of pre-eclampsia, maternal diabetes, maternal drug abuse, meconium-stained amniotic fluid or polycythemia. In that study, only three patients were healthy prior to development of NEC.5
Other studies have also confirmed the hypothesis that the occurrence of NEC in a full-term infant is usually associated with a predisposing event. Out of 29 full-term infants with NEC, Bolissety found only two that had no prior illness known to be associated with the development of NEC.3 Beeby reported eight full-term infants with NEC, all with a predisposing event.18 Similarly, Wiswell found an unremarkable course prior to the development of NEC in only three of 43 full-term infants with NEC.12 Our study shows only a 50% rate of infants with known risk factors for NEC. The other seven infants had no known risk factors for NEC, but still exhibited some minor medical conditions, such as asymptomatic hypoglycemia, mild tachypnea, hyperbilirubinemia requiring phototherapy, and delivery by CS with or without mild abnormal fetal heart monitoring and with no apparent birth asphyxia.
Several studies identified a connection between congenital heart disease and NEC in term infants. The frequency of this connection ranged from 7.6% to 38% of term infants with NEC: Polin — 5 out of 13,4 Thilo — 6 out of 79,6 Andrews — 2 out of 107 and Bolissety — 10 out of 29.3
To the best of our knowledge, only two cases of hypothyroidism and NEC have been described so far. The first was the case of a 10-day-old full-term infant with a history of hyperbilirubinemia requiring phototherapy. Positive clinical signs included persistent open posterior fontanelle. No thyroid tissue was identified by ultrasound. The infant was treated with intravenous thyroxin.19 The second patient developed NEC at the age of 6 weeks, 10 days after Nissen funduplication for severe gastro-esophageal reflux. Prior history included hypoxic–ischemic encephalopathy with seizures within the first 24 hours, treated with anticonvulsants. Thyroxin was commenced at age 17 days. Investigation confirmed thyroid dysmorphogenesis. Both infants were diagnosed by the newborn screening test,3 as was the case presented in our study. A pathogenic relationship between hypothyroidism and NEC has been suggested. Thyroid hormone deficiency causes decreased gut motility due to peripheral neuropathy of the intestine. In the presence of feeding, this may allow for intestinal bacterial overgrowth, increased gas production and abdominal distension. A second factor relating the hypothyroid state with NEC is the hemo-dynamic effect of thyroid hormone deficiency. In the fetal and perinatal periods, the thyroid hormone is required for normal increase in cardiac output in response to catecholamines. An unsatisfactory increase in cardiac output in response to stress may lead to decreased mesenteric blood flow and bowel ischemia.19
NEC in term infants has also been associated with the repair of gastroschisis8 and myelomeningocele and lipomyelomeningocele.10 The pathogenesis is unknown, but several factors appear to play either a primary or a secondary role, including infectious agents and toxins, enteral alimentation, exposure to anesthetic agents and mesenteric ischemia with tissue hypoxia.
The development of NEC most probably involves multiple factors in the setting of a stressed intestinal system with immature protective mechanisms. About 90% of NEC infants in the study group were receiving all of their meals by mouth prior to the development of NEC. It is hypothesized that (1) incompletely digested formula can provide a substrate for bacterial proliferation and (2) feeding increases intestinal oxygen demand during nutrient absorption, thus increasing the risk of intestinal tissue hypoxia that can cause mucosal injury and bacterial invasion. Most neonatologists increase feeding volumes gradually in preterm infants, although this is usually not the case for full-term infants. Human milk appears to be beneficial in preventing NEC, most probably by enhancing growth of lactobacilli and by immunologic mechanisms.1, 11 The infants in the study group were distinguished by a lack of sufficient breast milk.
For many years, mesenteric ischemia was postulated to be the common denominator in NEC. Cardiovascular stresses such as hypotension, hypothermia, hypoxia, feeding, anemia and umbilical vessel catheterization are all associated with the development of NEC. The immature intestines may have reduced ability to regulate blood flow and oxygenation.1
Bacterial colonization of the intestinal tract is a prerequisite for initiation of NEC. The occurrence of NEC in epidemics suggests that an infectious agent may play a role in the pathogenesis of NEC. Numerous bacteria and viruses have been isolated in epidemics, including Pseudomonas aeruginosa, E. coli, Klebsiela pneumonia, Clostridium perfringes, butyricum and difficile, Enteroviruses, Coxsackie B virus, Corona virus and Rotavirus. Nonetheless, most of these isolated organisms are part of the normal intestinal flora. Supplementation with Bifidobacterium infantis and Lactobacillus acidophilus reduced the incidence of NEC, probably by preventing the overgrowth of more pathogenic enterobacteria.1, 10, 11 This etiology could not explain the high incidence of NEC in the study infants described here.
Locally produced cytokines may have a detrimental effect during the evolvement of NEC. Other mechanisms are in place for downward regulation of this proinflammatory activation. A relative deficiency in protective responses may account for the propensity of intestinal injury in premature infants. The concentration of Interleukin 1 and 6 (IL-1, IL-6) and Tumor-Necrosis-Factor-alpha (alpha-TNF) is elevated locally. Nitric-oxide (NO) production by enterocytes is increased and results in enterocyte apoptosis through peroxy-nitrite formation. Conversely, NO deficiency may also predispose the intestine to NEC.10
Moreover, deficiencies in both magnesium and copper can damage the gut's antioxidative defense and produce a pro-NEC intestinal cytokine profile.10 The phospholipid inflammatory mediator, platelet-activating factor, has also been implicated in the pathogenesis of NEC. Erythropoietin is a trophic hormone that protects against intestinal cell death and was found to have a protective role, as did epidermal growth factor and hepatocyte growth factor.11
CONCLUSION
In conclusion, only half of our full-term infants exhibited any major known risk factors that predisposed them to NEC. The early onset of NEC both with and without any major risk factors might suggest a common mechanism related to a perinatal ischemic insult. Such an insult may compromise the intestinal blood supply without our ability at present to detect any sign of it prior to feeding initiation. The increasing rate of CS in our institution, together with the fact that all the study infants except one were born by CS, either elective or urgent, might suggest that CS plays a role in the pathogenesis of NEC. The etiology of the increasing number of full-term infants with NEC in our institution and the possible role of CS in its pathogenesis deserve further investigation.
References
Fanaroff AA, Martin RJ . Neonatal-Perinatal Medicine. 7th ed. Mosby: London, 2002. p. 1298–1300.
Behrman RE, Kliegman RM, Jenson HB . Nelson Textbook of Pediatrics. 16th ed, 2000. p. 512–513.
Bolissety S, Lui K, Oei J, Wojtulewicz J . A regional study of underlying congenital diseases in term neonates with necrotizing enterocolitis. Acta Paediatr 2000;89 (10):1226–1230.
Polin RA, Pollack PF, Barlow B, et al. Necrotizing enterocolitis in term infants. J Pediatr 1976;89 (3):460–462.
Martinez-Tallo E, Claure N, Bancalari E . Necrotizing enterocolitis in full-term or near-term infants: risk factors. Biol Neonate 1997;71 (5):292–298.
Thilo EH, Lazarte RA, Hernandez JA . Necrotizing enterocolitis in the first 24 hours of life. Pediatrics 1984;73 (4):476–480.
Andrews DA, Sawin RS, Ledbetter DJ, Schaller RT, Hatch EI . Necrotizing enterocolitis in term neonates. Am J Surg 1990;159 (5):507–509.
Oldham KT, Coran AG, Drongowski RA, Baker PJ, Wesley JR, Polley Jr TZ . The development of necrotizing enterocolitis following repair of gastroschisis: a surprisingly high incidence. J Pediatr Surg 1988;23 (10):945–949.
Bell MJ, Ternberg JL, Feigin RD, et al. Neonatal necrotizing enterocolitis. Therapeutic decisions based upon clinical staging. Ann Surg 1978;187 (1):1–7.
Ng S . Necrotizing enterocolitis in the full term neonate. J Paediatr Child Health 2001;37 (1):1–4.
Caplan MS, Jilling T . New concepts in necrotizing enterocolitis. Curr Opin Pediatr 2001;13 (2):111–115.
Wiswell TE, Robertson CF, Jones TA, Tuttle DJ . Necrotizing enterocolitis in full-term infants, a case–control study. Am J Dis Child 1988;142 (5):532–535.
Ruangtrakool R, Laohapensang M, Sathomkich C, Talalak P . Necrotizing enterocolitis: a comparison between full-term and pre-term neonates. J Med Assoc Thai 2001;84 (3):323–331.
Kabeer A, Gunnlaugsson S, Coren C . Neonatal necrotizing enterocolitis. A 12 year review at a country hospital. Dis Colon Rectum 1995;38 (8):866–872.
Uauy RD, Fanaroff AA, Korones SB, Phillips EA, Wrigh LL . Necrotizing enterocokitis in very low birth weight infants: biodemographic and clinical correlates. National Institute of Child Health and Human Development Neonatal Research Network. J Pediatr 1991;119 (4):630–638.
Minkoff H, Chervenak FA . Elective primary cesarean delivery. N Engl J Med 2003;348 (10):946–950.
Sweet DG, Craig B, Halliday HL, Mulholland C . Gastro-intestinal complications following neonatal cardiac catheterization. J Perinatol Med 1998;26 (3):196–200.
Beeby PJ, Jeffery H . Risk factors for necrotizing enterocolitis: the influence of gestational age. Arch Dis Child 1992;67 (4):432–435.
Amer T, David R, Oberfield SE . Necrotizing enterocolitis and hypothyroidism in a newborn infant: treatment with intravenous L-thyroxin. Am J Perinatol 1994;11 (1):30–32.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Maayan-Metzger, A., Itzchak, A., Mazkereth, R. et al. Necrotizing Enterocolitis in Full-Term Infants: Case–Control Study and Review of the Literature. J Perinatol 24, 494–499 (2004). https://doi.org/10.1038/sj.jp.7211135
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.jp.7211135
This article is cited by
-
To feed or not to feed during therapeutic hypothermia in asphyxiated neonates: a systematic review and meta-analysis
European Journal of Pediatrics (2023)
-
Development of necrotizing enterocolitis in full-term infants with duct dependent congenital heart disease
BMC Pediatrics (2022)
-
Challenges in diagnosing necrotizing enterocolitis
Pediatric Research (2020)
-
Necrotizing Enterocolitis in Infants with Hypoplastic Left Heart Syndrome Following Stage 1 Palliation or Heart Transplant
Pediatric Cardiology (2018)
-
Differences in the Clinical Characteristics of Early- and Late-Onset Necrotizing Enterocolitis in Full-Term Infants: A Retrospective Case-Control Study
Scientific Reports (2017)