Abstract
Objective:
Little information exists regarding gastric residual (GR) evaluation prior to feedings in premature infants. The purpose of this study was to compare the amount of feedings at 2 and 3 weeks of age, number of days to full feedings, growth and incidence of complications between infants who underwent RGR (routine evaluation of GR) evaluation versus those who did not.
Study Design:
Sixty-one premature infants were randomized to one of two groups. Group 1 received RGR evaluation prior to feeds and Group 2 did not.
Result:
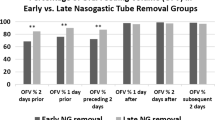
There was no difference in amount of feeding at 2 (P=0.66) or 3 (P=0.41) weeks of age, growth, days on parenteral nutrition or complications. Although not statistically significant, infants without RGR evaluation reached feeds of 150 ml kg−1 per day 6 days earlier and had 6 fewer days with central venous access.
Conclusion:
Results suggest RGR evaluation may not improve nutritional outcomes in premature infants.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Jadcherla SR, Kliegman RM . Studies of feeding intolerance in very low birth weight infants: definition and significance. Pediatrics 2002; 109 (3): 516–517.
Meetz WH, Valentine C, McGuigan JE, Conlon M, Sacks N, Neu J . Gastrointestinal priming prior to full enteral nutrition in very low birth weight infants. J Pediatr Gastroent Nutr 1992; 15 (2): 163–170.
Mihatsch WA, von Schoenaich P, Fahnenstich H, Dehne N, Ebbecke H, Plath C . The significance of gastric residuals in the early enteral feeding advancement of extremely low birth weight infants. Pediatrics 2002; 109 (3): 457–459.
Cobb BA, Carlo WA, Ambalavanan N . Gastric residuals and their relationship to necrotizing enterocolitis in very low birth weight infants. Pediatrics 2004; 113 (1 Pt 1): 50–53.
Flidel-Rimon O, Branski D, Shinwell ES . The fear of necrotizing enterocolitis versus achieving optimal growth in preterm infants—an opinion. Acta Paediatr. 2006; 95 (11): 1341–1344.
Kliegman RM . Experimental validation of neonatal feeding practices. Pediatrics 1999; 103 (2): 492–493.
Neu J . Is it time to stop starving premature infants? J Perinatol 2009; 29 (6): 399–400.
Torrazza RM, Neu J . Evidence-based guidelines for optimization of nutrition for the very low birthweight infant. Neo Rev 2013; 14 (7): e340–e349.
Goldstein B, Giroir B, Randolph A International Consensus Conference on Pediatrics. International pediatric sepsis consensus conference: definitions for sepsis and organ dysfunction in pediatrics. Pediatric Critical Care Medicine: a Journal of the Society of Critical Care Medicine and the World Federation of Pediatric Intensive and Critical Care Societies 2005; 6 (1): 2–8.
Stephens BE, Walden RV, Gargus RA, Tucker R, McKinley L, Mance M et al. First-week protein and energy intakes are associated with 18-month developmental outcomes in extremely low birth weight infants. Pediatrics 2009; 123 (5): 1337–1343.
Kuschel CA, Harding JE . Multicomponent fortified human milk for promoting growth in preterm infants. Cochrane Database Syst Rev 2004; (1): CD000343.
Riezzo G, Indrio F, Montagna O, Tripaldi C, Laforgia N, Chiloiro M et al. Gastric electrical activity and gastric emptying in term and preterm newborns. Neurogastroenterol Motil. 2000; 12 (3): 223–229.
Lau C, Smith EO, Schanler RJ . Coordination of suck-swallow and swallow respiration in preterm infants. Acta Paediatr 2003; 92 (6): 721–727.
Omari TI, Barnett C, Snel A, Goldsworthy W, Haslam R, Davidson G et al. Mechanisms of gastroesophageal reflux in healthy premature infants. J Pediatr 1998; 133 (5): 650–654.
Liang J, Co E, Zhang M, Pineda J, Chen JD . Development of gastric slow waves in preterm infants measured by electrogastrography. Am J Physiol 1998; 274 (3 Pt 1): 503–508.
Berseth CL . Gestational evolution of small intestine motility in preterm and term infants. J Pediatr 1989; 115 (4): 646–651.
Shulman RJ, Ou C-N, Smith EOB . Evaluation of potential factors predicting attainment of full gavage feedings in preterm infants. Neonatology 2010; 99 (1): 38–44.
Parker LA, Neu J, Torrazza RM, Li Y . Scientifically based strategies for enteral feeding in premature infants. Neo Rev 2013; 14 (7): e350–e359.
Bertino E, Giuliani F, Prandi G, Coscia A, Martano C, Fabris C . Necrotizing enterocolitis: risk factor analysis and role of gastric residuals in very low birth weight infants. J Pediatr Gastroenterol Nutr 2009; 48 (4): 437–442.
Cole CR, Hansen NI, Higgins RD, Bell EF, Shankaran S, Laptook AR et al. Bloodstream infections in very low birth weight infants with intestinal failure. J Pediatr 2012; 160 (1): 54–59 e52.
Acknowledgements
Dr Murgas’s work was funded by a Gerber Foundation Novice Research Grant. Dr Parker’s work has been funded by the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
Dr Neu claims disclosures but no conflict of interest. Disclosures include Scientific Advisory Panel: Medela and Mead Johnson, Consultant: Infant Microbial Therapeutics, Lecturer: Nestle, Abbott, Mead Johnson, and Danone. Drs Li, Shuster, Neu and Beth Talaga declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Torrazza, R., Parker, L., Li, Y. et al. The value of routine evaluation of gastric residuals in very low birth weight infants. J Perinatol 35, 57–60 (2015). https://doi.org/10.1038/jp.2014.147
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2014.147
This article is cited by
-
Routine prefeed gastric aspiration in preterm infants: a systematic review and meta-analysis
European Journal of Pediatrics (2021)
-
Is routine evaluation of gastric residuals for premature infants safe or effective?
Journal of Perinatology (2020)
-
Very low birth weight infants receive full enteral nutrition within 2 postnatal weeks
Journal of Perinatology (2020)
-
Reducing time to initiation and advancement of enteral feeding in an all-referral neonatal intensive care unit
Journal of Perinatology (2018)