Abstract
Background
Neurologic complications in neonates supported with extracorporeal membrane oxygenation (ECMO) are common and diminish their quality of life and survival. An understanding of factors associated with neurologic complications in neonatal ECMO is lacking. The goals of this study were to describe the epidemiology and factors associated with neurologic complications in neonatal ECMO.
Patients and methods
Retrospective cohort study of neonates (age ≤30 days) supported with ECMO using data reported to the Extracorporeal Life Support Organization during 2005–2010.
Results
Of 7,190 neonates supported with ECMO, 1,412 (20 %) had neurologic complications. Birth weight <3 kg [odds ratio (OR): 1.3; 95 % confidence intervals (CI): 1.1–1.5], gestational age (<34 weeks; OR 1.5, 95 % CI 1.1–2.0 and 34–36 weeks: OR 1.4, 95 % CI 1.1–1.7), need for cardiopulmonary resuscitation prior to ECMO (OR 1.7, 95 % CI 1.5–2.0), pre-ECMO blood pH ≤ 7.11 (OR 1.7, 95 % CI 1.4–2.1), pre-ECMO bicarbonate use (OR 1.3, 95 % CI 1.2–1.5), prior ECMO exposure (OR 2.4, 95 % CI 1.6–2.6), and use of veno-arterial ECMO (OR 1.7, 95 % CI 1.4–2.0) increased neurologic complications. Mortality was higher in patients with neurologic complications compared to those without (62 % vs. 36 %; p < 0.001).
Conclusions
Neurologic complications are common in neonatal ECMO and are associated with increased mortality. Patient factors, pre-ECMO severity of illness, and use of veno-arterial ECMO are associated with increased neurologic complications. Patient selection, early ECMO deployment, and refining ECMO management strategies for vulnerable populations could be targeted as areas for improvement in neonatal ECMO.
Similar content being viewed by others
Introduction
Neurologic complications are common during extracorporeal membrane oxygenation (ECMO) and are associated with increased mortality and long-term morbidity [1–6]. Neurologic complications during ECMO may be related to patient characteristics, pre-ECMO severity of illness, ECMO management, and complications during ECMO [3–5]. The incidence and factors associated with neurologic complications during ECMO in specific populations such as children supported with ECMO for cardiac arrest (ECPR) have been previously reported [2, 7, 8]. Brain immaturity increases vulnerability to neurologic complications for neonates supported with ECMO. Hardart et al. [9, 10] previously reported that intracranial hemorrhage (ICH) occurred in 9.9 % of neonates supported with ECMO. They also reported that ICH in this population was associated with gestational age, diagnosis of sepsis, severe metabolic acidosis, use of epinephrine, and coagulopathy prior to ECMO deployment. Since this report in 1998, indications for use of ECMO in the neonatal population has changed, with fewer neonates supported for respiratory and more for cardiac indications [11]. In addition, ECMO technology has changed, and experience in the management of ECMO patients has improved. The impact of these issues on the incidence and risk factors for neurologic complications in newborns supported with ECMO has not been evaluated. New information on the incidence and factors associated with neurologic complications in neonates supported with ECMO may be useful in planning interventions that can help reduce these complications and improve ECMO outcomes.
The goals of this study were to determine the incidence of neurologic complications and to identify patient demographic, pre-ECMO, and ECMO support-related variables associated with neurologic complications using a recent multicenter cohort of neonates supported with ECMO for all indications.
Materials and methods
Data for purposes of this study were obtained from the ECMO registry of the Extracorporeal Life Support Organization (ELSO). The ECMO registry collects data on ECMO used to support cardiorespiratory function in newborns, children, and adults. Registry data are reported from approximately 230 member centers including US and international centers after approval through local institutional review boards. An agreement between member centers and ELSO allows the release of limited de-identified data sets for purposes of research without the need for further approval from individual centers. Data are reported to the registry from the contributing centers using a standardized data sheet containing patient demographics, diagnosis, ECMO indication and support details, and patient outcomes. For this study, data from all neonates (≤30 days of age at ECMO deployment) reported to the ECMO registry during the calendar years 2005–2010 were extracted.
Definition of neurologic complications
Neurologic complications were defined as brain death, cerebral infarction, intracranial hemorrhage (ICH), or seizures [1, 2] diagnosed during ECMO support and identified using ELSO registry neurologic complication codes. Cerebral infarction and ICH reported to the registry were diagnosed using head ultrasound (HUS) or computerized tomography imaging of the head. Seizures were diagnosed clinically or using an electroencephalogram (EEG). Time to diagnosis of a neurologic event after ECMO deployment, long-term follow-up, and functional outcome data were not collected by the registry and could not be used to further characterize the severity of neurologic complications.
Variables for analysis
Variables used included: patient age, diagnosis, type and duration of ECMO support, number of ECMO runs per patient, pre-ECMO mechanical ventilator settings, patient support details, worst blood gas values obtained within the 6 h prior to ECMO initiation, and in-hospital mortality. Pre-ECMO cardiac arrest was defined as cardiac arrest requiring cardiopulmonary resuscitation occurring from the time of admission but prior to initiation of ECMO. Decisions regarding patient selection, patient management before, on, or after ECMO, and the use of imaging for assessment of neurologic injury were not standardized across the reporting institutions and were subject to practice variability. In addition, data regarding anticoagulation management were not collected by ELSO and were unavailable for analysis.
Data categorization
Primary and Secondary International Classification of Diseases, 9th edition (ICD-9), diagnosis codes reported to the registry were used to create the diagnostic categories including “congenital heart disease (CHD),” “congenital diaphragmatic hernia (CDH),” “persistent pulmonary hypertension of the newborn (PPHN),” “meconium aspiration syndrome (MAS),” “respiratory distress syndrome (RDS),” “respiratory infection,” “sepsis,” and “other,” containing patients that could not be assigned to one of the above groups. Primary indication for ECMO included “pulmonary,” “cardiac,” and “ECPR” based on definitions created by the ECMO registry. Patients were categorized as cannulated through the neck if either the internal jugular vein or carotid artery was one of the cannulation sites reported. Patients were assigned as cannulated through the chest if either the right atrium or aorta was used for cannulation.
Statistical Analysis
For patients (n = 215) who had more than one ECMO run, only data from the last run were included for analysis. Demographic, pre-ECMO, and ECMO support details at the time of ECMO initiation were compared for patients with or without neurologic complications using the Mann-Whitney U test for continuous data and the chi-square test for categorical data. The Fisher’s exact test was used when expected counts in >20 % of cells were <5. A chi-square test for linear trend was used to study trends in the incidence of neurologic injury over the study time period.
Multivariable logistic regression was used to explore the association of variables related to demographic, pre-ECMO, and ECMO support obtained at the time of ECMO deployment and neurologic complications during ECMO. Candidate variables for inclusion in the multivariable models were chosen from the univariate analysis with criteria for variable selection set at a p value <0.1. A backward selection procedure was used for entry of variables into the model, and variables were retained if their adjusted p value was <0.05.
Because diagnostic groups and the indication for ECMO, pre-ECMO arterial blood pH, and pCO2, and neck and chest cannulation for ECMO were collinear variables, only the indication for ECMO, arterial blood pH, and neck cannulation were considered for inclusion in the model as data. Variables with data missing from >10 % of cases were not considered for inclusion in the model to prevent loss of information. Subjects with missing values from one or more independent variables were excluded from inclusion in the multivariable model. Continuous variables [e.g., weight at ECMO, gestational age (GA), pre-ECMO arterial blood pH] retained in the logistic regression model were refitted as categorical variables to allow for possible non-linear association with the outcome. Continuous variables were categorized as tertiles or quartiles of their distribution. SPSS version 18.0 software (SPSS, Chicago, IL) was used for the analysis. Data are reported as frequency (n) with proportion (%), median values with interquartile range (IQR: 25th, 75th percentile), or odds ratios (OR) with 95 % confidence intervals (CI). Statistical significance was set at p <0.05.
Results
Study population
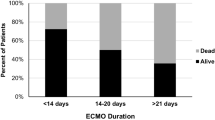
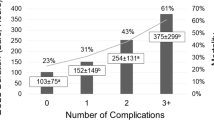
A total of 7,405 ECMO runs in 7,190 neonates were reported to the ECMO registry during the study period. Median age at ECMO was 2 days (IQR 1, 7), 56 % of the patients were male, and 53 % of the patients were white race. Congenital heart disease (n = 2,368, 33 %), meconium aspiration syndrome (n = 1,474, 21 %), congenital diaphragmatic hernia (n = 1,468, 20 %), and persistent pulmonary hypertension of the newborn (n = 1,371, 19 %) were the most common diagnostic categories. Indications for ECMO included respiratory failure (n = 4,787, 66 %), cardiac disease (n = 1,903, 27 %), and ECMO to aid cardiopulmonary resuscitation (ECPR; n = 500, 7 %). The median duration of ECMO was 141 (IQR: 88, 238) hours. The incidence and types of neurological complications are shown in Table 1. A single neurologic complication code was present in 1,219 neonates (17 %), whereas multiple codes were present in 203 (3 %) neonates. The incidence of neurologic complications in ECMO neonates did not vary by year (chi-square for linear trend, p = 0.2). Mortality prior to hospital discharge was higher in those with compared to those without neurologic complications (62 vs. 36 %; p < 0.001).
Comparison of patients with and without neurologic complications
Demographic information
Table 1 shows demographic features of neonates with and without neurologic complications during ECMO. Neonates with neurologic complications had lower GA and body weight than those without. Diagnostic category and indication for ECMO support were significantly different between the two groups. Neurologic complications were lowest among neonates whose indication for ECMO was respiratory failure compared to cardiac and ECPR indications. Similarly, neonates supported with ECMO for meconium aspiration syndrome (13 %), respiratory distress syndrome of the newborn (16 %), and PPHN (17 %) had a lower incidence of neurologic complications compared to those with sepsis (33 %), congenital heart disease (22 %), and classified as the miscellaneous group (26 %). Neurologic complications were higher among neonates whose gestation age was ≤36 weeks compared to term or post-term neonates. The distribution of neurologic complications based on weight and GA is shown in Fig. 1.
Pre-ECMO and ECMO support data
Pre-ECMO and ECMO details of neonates with and without neurologic complications are shown in Table 2. Neurologic complications occurred more frequently in patients treated with surfactant and intravenous bicarbonate. Pre-ECMO blood gas values for pH, partial pressure of oxygen (PaO2), standardized bicarbonate level, and peripheral oxygen saturation (SaO2) were significantly lower, and partial pressure of carbon dioxide was significantly higher in neonates with neurologic complications. ECMO cannulation sites and duration of ECMO support were similar for the two groups (Table 3).
Multivariable model of factors associated with neurologic complications during ECMO
Factors associated with neurologic complications in neonates supported with ECMO are shown in Table 4. Neonates with lower birth weight (<3 kg compared to >3.5 kg), lower GA [very preterm (<34 weeks GA) and preterm (34–36 weeks GA) compared to term neonates (39–40 weeks GA)], those with prior exposure to ECMO, and those supported with veno-arterial (VA) ECMO had increased odds of neurologic complications. Similarly, those with a cardiac arrest requiring CPR and bicarbonate replacement prior to ECMO had increased odds of neurologic complications. Finally, those with low arterial blood gas pH (≤7.11 compared to pH ≥7.34) obtained within the 6 h prior to ECMO cannulation had increased odds of neurologic complications.
Discussion
In our cohort of neonates supported with ECMO, we found that neurologic complications were common and occurred in 20 % of the subjects. The most frequent form of neurologic injury was ICH. We found that prematurity, lower body weight, cardiac arrest, and severe physiological instability before ECMO deployment increased the odds of neurologic complications.
In neonatal ECMO, factors present prior to and during ECMO support have been shown to be associated with brain injury [4, 5, 12] In laboratory animals, severe hypoxemia similar to that seen in neonatal respiratory failure has been shown to alter cerebral autoregulation, resulting in increased vulnerability of the cerebral circulation to ischemia during systemic hypotension, and hyperemia with hypertension [4, 13–15]. When cerebral blood flow has been restored after exposure to hypoxemia with ECMO flow, the cerebral circulation may be exposed to higher blood pressure, leading to cerebral hyperemia and ICH. The duration of hypoxemia before autoregulation is lost is unclear. In animal models, it has been shown that loss of autoregulation occurs even after brief exposure to hypoxemia and that cerebral autoregulation remains altered for several hours after restoration of gas exchange and circulation. Based on these animal studies, it appears that increased vulnerability to ICH may be present prior to and immediately following ECMO deployment.
Similar mechanisms may be in play in neonates supported with ECMO. Clinical investigations in neonatal ECMO have shown that the severity of cardiopulmonary dysfunction prior to ECMO, indicated by severe metabolic acidosis, cardiac arrest, or epinephrine use prior to ECMO cannulation, was associated with an increased incidence of ICH [9, 10, 16–18]. Our findings of increased odds of neurologic complications in neonates with low arterial blood pH, those requiring bicarbonate replacement, and those with cardiac arrest prior to ECMO support the notion that severity of illness prior to ECMO may increase the risk of neurologic injury. Thus, early deployment of ECMO prior to the onset severe metabolic acidosis or cardiac arrest may prevent neurologic injury in some cases.
Investigations on the timing of ICH in neonates supported with ECMO have shown that ICH commonly occurs within the first 72 h after ECMO deployment [16, 19]. Thus, neonates supported with ECMO for severe cardiopulmonary dysfunction may require increased vigilance during this period. In a cohort of neonates supported with ECMO, Khan et al. [19] reported that 19 % had ICH on HUS prior to ECMO deployment. Thus, in some cases, ICH can occur before ECMO deployment and can be worsened by ECMO use. Screening HUS prior to ECMO deployment may be useful for identifying pre-existing ICH so ECMO management can be modified to decrease ICH extension. However, obtaining a screening HUS may not always be practical, as ECMO is often required emergently and cannot be delayed to obtain a screening HUS.
Prior studies have found neonates with illness associated with coagulopathy such as sepsis had increased ICH during ECMO [9, 17, 20]. Heparin anticoagulation used for the conduct of ECMO confers additional risk of ICH in these patients. Wilson et al. [21] in a series of neonates supported with ECMO showed that the incidence of ICH was decreased in patients treated with fibrin-stabilizing agents such as epsilon amino caproic acid (Amicar) during ECMO. However, in a more recent report, the use of epsilon amino caproic acid (Amicar) during neonatal ECMO was shown to decrease surgical bleeding but not ICH [22]. These authors suggested that in neonates at higher risk of bleeding complications on ECMO, namely those with severe hypoxia, severe metabolic acidosis, ICH, and coagulopathy prior to ECMO, and premature newborns, use of fibrin stabilizing agents may reduce bleeding complications, including ICH. The efficacy of epsilon amino caproic acid in preventing ICH in neonates supported with ECMO has not been tested in a randomized controlled trial to support its routine use.
Neurologic injury may occur as a result of the cannulation of the carotid artery and internal jugular vein used to conduct ECMO [5, 13, 23]. Prior studies have shown that both cerebral blood flow and EEG rhythm were maintained after ligation of the carotid artery during ECMO cannulation [24, 25]. Although we did not show increased neurologic complications in neonates cannulated using the neck vessels, we found that patients supported with VA compared to VV-ECMO had increased neurological complications. Loss of pulsatile cerebral blood flow, decreased cerebral autoregulation, and circuit-associated emboli during VA ECMO may explain the increased neurologic injury rate in neonates supported with VA ECMO [4, 5, 13, 23]. Alternatively, increased neurologic complications in VA ECMO may merely reflect more severe cardiorespiratory dysfunction, conferring a higher risk of neurologic complications in VA ECMO patients. Thus, in neonates with respiratory failure, but with preserved cardiac function requiring ECMO, use of VV instead of VA ECMO may lower the incidence of neurologic injury.
Many centers consider prematurity a contraindication for ECMO support in neonates because of the increased risk of ICH in this population [10, 26]. Both prematurity (GA <36 weeks) and lower weight (<3 kg) were associated with increased neurologic complications in our cohort. Increased propensity to neurologic injury in premature infants may be mediated by cellular and molecular maturation-dependent mechanisms. Premature neonates on ECMO are at high risk of ICH due to the presence of a friable germinal matrix with poor supporting stroma [27, 28]. Hemodynamic instability, fluctuations in cerebral blood flow, and exposure to anticoagulation may compound this risk. Since an increasing number of premature neonates is being considered for ECMO support, better understanding of ECMO and anticoagulation management in these neonates is needed. Finally, we found an association between the need for multiple ECMO runs and neurologic complications [29]. Continued hemodynamic instability after successful ECMO decannulation, re-exposure to anticoagulation therapies, and subtle neurologic injury acquired during the prior ECMO exposure may explain the increased incidence of neurologic complications in this subset. Although exposure to a second run of ECMO may be lifesaving in some situations, it is important to consider the increased risk of neurologic complications in clinical decision making and when providing information to families.
We found the incidence of non-hemorrhagic neurologic complications such as cerebral infarction, seizures, and brain death to be low compared to ICH. Cerebral infarction can occur as a result of emboli from the ECMO circuit. Embolic cerebral infarcts are at risk of hemorrhagic conversion when the anticoagulation is started and are often the nidus for ICH [5]. Ischemic brain injury may occur prior to ECMO at a time when cerebral autoregulation is impaired. Need for cardiopulmonary resuscitation prior to ECMO cannulation increases the incidence of neurologic complications including ischemic brain injury in ECMO patients of all ages [1, 2]. We found higher odds of neurologic complications in newborns requiring pre-ECMO CPR. These findings again illustrate that early recognition of the need for ECMO support and ECMO deployment before cardiac arrest may help reduce the incidence of neurologic injury. Therapeutic hypothermia has been shown to reduce death and neurological disability in neonates after cardiac arrest and is used in many centers to improve neurologic outcomes in neonates with birth asphyxia and cardiac arrest [30, 31]. The potential role of therapeutic hypothermia in improving neurologic outcomes in neonatal ECMO has not been previously studied and should be investigated in the future.
Limitations of our data set and our definition of neurological injury require careful consideration when interpreting the data presented here. Data are reported to the ELSO registry on a voluntary basis and are therefore subject to reporting bias, so neurologic complications may be underreported. The data analyzed here were not specifically collected for studying neurologic complications in neonates supported with ECMO. We included seizures, including those diagnosed clinically in our definition of neurological injury. Clinical diagnosis of seizures is subject to misinterpretation; seizures may not be entirely attributable to ECMO use and may not be associated with underlying neurological injury [32, 33]. Information on the severity of neurologic injury was not collected and could not be used to classify neurologic complications. We cannot determine the timing of neurologic injury, and thus some patients in our cohort may have had injury prior to the initiation of ECMO. Data regarding the presence of coagulation disorders and anticoagulation management were not available for studying the influence of these important issues on neurologic complications during ECMO. Finally, important information on functional outcomes and quality of life in survivors with neurologic complications was not available for analysis.
Despite these many limitations, we can say that neurologic complications are common in neonates supported with ECMO and that a high-risk cohort of neonates can be identified. Premature neonates, weight < 3 kg, support with VA ECMO, those re-cannulated after prior ECMO exposure, those with severe acidosis, and those with pre-ECMO cardiac arrest requiring CPR may be at higher risk for neurologic complications during ECMO. In these high-risk neonates, whether early ECMO deployment, modification of existing ECMO management protocols, neurologic imaging, anticoagulation management, and early use of neuro-protective therapies can decrease neurologic complications should be investigated in the future.
References
Cengiz P, Seidel K, Rycus PT, Brogan TV, Roberts JS (2005) Central nervous system complications during pediatric extracorporeal life support: incidence and risk factors. Crit Care Med 33:2817–2824
Barrett CS, Bratton SL, Salvin JW, Laussen PC, Rycus PT, Thiagarajan RR (2009) Neurological injury after extracorporeal membrane oxygenation use to aid pediatric cardiopulmonary resuscitation. Pediatr Crit Care Med 10:445–451
Bulas D, Glass P (2005) Neonatal ECMO: neuroimaging and neurodevelopmental outcome. Semin Perinatol 29:58–65
Short BL (2005) The effect of extracorporeal life support on the brain: a focus on ECMO. Semin Perinatol 29:45–50
Volpe JJ (2008) Intracranial Hemorrhage: Subdural, Primary Subarachanoid, Cerebral, Intraventricular (Term Infant) and Miscellaneous. In: Volpe JJ (ed) Neurology of the newborn. Saunders Elsevier, Philadelphia, pp 483–516
Hervey-Jumper SL, Annich GM, Yancon AR, Garton HJ, Muraszko KM, Maher CO (2011) Neurological complications of extracorporeal membrane oxygenation in children. J Neurosurg Pediatr 7:338–344
Thiagarajan RR, Laussen PC, Rycus PT, Bartlett RH, Bratton SL (2007) Extracorporeal membrane oxygenation to aid cardiopulmonary resuscitation in infants and children. Circulation 116:1693–1700
Sivarajan VB, Best D, Brizard CP, Shekerdemian LS, d’Udekem Y, Butt W (2011) Duration of resuscitation prior to rescue extracorporeal membrane oxygenation impacts outcome in children with heart disease. Intensive Care Med 37:853–860
Hardart GE, Fackler JC (1999) Predictors of intracranial hemorrhage during neonatal extracorporeal membrane oxygenation. J Pediatr 134:156–159
Hardart GE, Hardart MK, Arnold JH (2004) Intracranial hemorrhage in premature neonates treated with extracorporeal membrane oxygenation correlates with conceptional age. J Pediatr 145:184–189
Conrad SA, Rycus P (2012) The registry of the extracorporeal life support organization. In: Annich GM, Lynch WR, MacLaren G, Wilson JM, Bartlett RH (eds) ECMO: extracorporeal cardiopulmonary support in critical care. Extracorporeal Life Support Organization, Ann Arbor, pp 87–104
Graziani LJ, Gringlas M, Baumgart S (1997) Cerebrovascular complications and neurodevelopmental sequelae of neonatal ECMO. Clin Perinatol 24:655–675
Short BL, Bender K, Walker LK, Traystman RJ (1994) The cerebrovascular response to prolonged hypoxia with carotid artery and jugular vein ligation in the newborn lamb. J Pediatr Surg 29:887–891
Short BL, Walker LK, Traystman RJ (1994) Impaired cerebral autoregulation in the newborn lamb during recovery from severe, prolonged hypoxia, combined with carotid artery and jugular vein ligation. Crit Care Med 22:1262–1268
Tweed A, Cote J, Lou H, Gregory G, Wade J (1986) Impairment of cerebral blood flow autoregulation in the newborn lamb by hypoxia. Pediatr Res 20:516–519
Biehl DA, Stewart DL, Forti NH, Cook LN (1996) Timing of intracranial hemorrhage during extracorporeal life support. ASAIO J 42:938–941
Dela Cruz TV, Stewart DL, Winston SJ, Weatherman KS, Phelps JL, Mendoza JC (1997) Risk factors for intracranial hemorrhage in the extracorporeal membrane oxygenation patient. J Perinatol 17:18–23
Grayck EN, Meliones JN, Kern FH, Hansell DR, Ungerleider RM, Greeley WJ (1995) Elevated serum lactate correlates with intracranial hemorrhage in neonates treated with extracorporeal life support. Pediatrics 96:914–917
Khan AM, Shabarek FM, Zwischenberger JB, Warner BW, Cheu HW, Jaksic T, Goretsky MJ, Meyer TA, Doski J, Lally KP (1998) Utility of daily head ultrasonography for infants on extracorporeal membrane oxygenation. J Pediatr Surg 33:1229–1232
Meyer DM, Jessen ME (1995) Results of extracorporeal membrane oxygenation in neonates with sepsis. The extracorporeal life support organization experience. J Thorac Cardiovasc Surg 109:419–425 Discussion 425–427
Wilson JM, Bower LK, Fackler JC, Beals DA, Bergus BO, Kevy SV (1993) Aminocaproic acid decreases the incidence of intracranial hemorrhage and other hemorrhagic complications of ECMO. J Pediatr Surg 28:536–540 Discussion 540–531
Downard CD, Betit P, Chang RW, Garza JJ, Arnold JH, Wilson JM (2003) Impact of AMICAR on hemorrhagic complications of ECMO: a ten-year review. J Pediatr Surg 38:1212–1216
Rollins MD, Hubbard A, Zabrocki L, Barnhart DC, Bratton SL (2012) Extracorporeal membrane oxygenation cannulation trends for pediatric respiratory failure and central nervous system injury. J Pediatr Surg 47:68–75
Perlman JM, Altman DI (1992) Symmetric cerebral blood flow in newborns who have undergone successful extracorporeal membrane oxygenation. Pediatrics 89:235–239
Lohrer RM, Bejar RF, Simko AJ, Moulton SL, Cornish JD (1992) Internal carotid artery blood flow velocities before, during, and after extracorporeal membrane oxygenation. Am J Dis Child 146:201–207
Rozmiarek AJ, Qureshi FG, Cassidy L, Ford HR, Gaines BA, Rycus P, Hackam DJ (2004) How low can you go? Effectiveness and safety of extracorporeal membrane oxygenation in low-birth-weight neonates. J Pediatr Surg 39:845–847
Back SA, Riddle A, McClure MM (2007) Maturation-dependent vulnerability of perinatal white matter in premature birth. Stroke 38:724–730
Volpe JJ (2008) Intracranial Hemorrhage: germinal matrix—intraventricular hemorrhage of the premature infant. In: Volpe JJ (ed) Neurology of the newborn. Saunders Elsevier, Philadelphia, pp 517–588
Meehan JJ, Haney BM, Snyder CL, Sharp RJ, Acosta JM, Holcomb GW 3rd (2002) Outcome after recannulation and a second course of extracorporeal membrane oxygenation. J Pediatr Surg 37:845–850
Shankaran S, Laptook AR, Ehrenkranz RA, Tyson JE, McDonald SA, Donovan EF, Fanaroff AA, Poole WK, Wright LL, Higgins RD, Finer NN, Carlo WA, Duara S, Oh W, Cotten CM, Stevenson DK, Stoll BJ, Lemons JA, Guillet R, Jobe AH (2005) Whole-body hypothermia for neonates with hypoxic-ischemic encephalopathy. N Engl J Med 353:1574–1584
Azzopardi DV, Strohm B, Edwards AD, Dyet L, Halliday HL, Juszczak E, Kapellou O, Levene M, Marlow N, Porter E, Thoresen M, Whitelaw A, Brocklehurst P (2009) Moderate hypothermia to treat perinatal asphyxial encephalopathy. N Engl J Med 361:1349–1358
Murray DM, Boylan GB, Ali I, Ryan CA, Murphy BP, Connolly S (2008) Defining the gap between electrographic seizure burden, clinical expression and staff recognition of neonatal seizures. Arch Dis Child Fetal Neonatal Ed 93:F187–F191
Clancy RR, McGaurn SA, Wernovsky G, Gaynor JW, Spray TL, Norwood WI, Jacobs ML, Goin JE (2003) Risk of seizures in survivors of newborn heart surgery using deep hypothermic circulatory arrest. Pediatrics 111:592–601
Conflicts of interest
The authors have no conflicts of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
Additional information
The authors have no financial relationships relevant to this article to disclose.
Rights and permissions
About this article
Cite this article
Polito, A., Barrett, C.S., Wypij, D. et al. Neurologic complications in neonates supported with extracorporeal membrane oxygenation. An analysis of ELSO registry data. Intensive Care Med 39, 1594–1601 (2013). https://doi.org/10.1007/s00134-013-2985-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-013-2985-x